What is Anti Mullerian Hormone and Why Does It Matter?
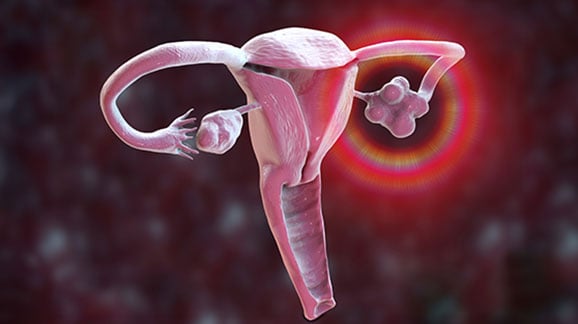
It is common to know anti mullerian hormone is the hormone which exhibits paramount importance while the topic of reproductive health is discussed especially regarding women. It is synthesised by the small follicles in ovaries; AMH is often applied to indicate the ovarian reserve which means the number of viable oocytes in the woman’s ovaries. Knowledge of AMH levels remains important to fertility which is why it is of great importance for those who have different plans regarding conception, those who have undergone certain fertility treatments, as well as for those who have some problems with their reproductive systems.
What is the Anti Mullerian hormone test?
Anti mullerian hormone is a protein hormone secreted by the granulosa cells which are encompassed by ovarian follicles. AMH has a role in controlling the growth of follicles and ensuring that follicle production is not done prematurely hence ensuring that a woman has a steady supply of eggs. Because AMH is secreted directly by these follicles, blood levels of AMH reflect the ovarian reserve.
Like most hormone concentrations, AMH is tested through a blood sample and, unlike most fertility biomarkers, it does not fluctuate in the menstrual cycle. This makes it possible to quantify it at any stage of the cycle, unlike the other hormones such as oestrogen that vary.
Why is AMH Important for Fertility?
In women, fertility is therefore associated with the number and quality of eggs they possess. From here, one can deduce that over time as women age their ovarian reserve decreases in number. This leads to a reduction in the number of eggs which are in the ovaries and the eggs that are in the ovaries may not be of the best quality as it was before. AMH stands for Anti Mullerian Hormone and indicates the picture, which shows how many eggs are left which can be fertilised.
Ladies with higher AMH levels also have more eggs compared to those who have low anti mullerian hormone levels which indicates that they have few eggs. Such information is essential for females involved in natural conception or through ART (assisted reproductive technologies) such as IVF (In Vitro Fertilisation).
What Are Normal AMH Levels?
It is also important to note that the AMH levels differ greatly from one woman to the other and depend on factors such as age, health among others and genetics. AMH does not have a standard reference value of ‘normal’ but there is an accepted cut-off that gives a rough idea of ovarian reserve. The AMH normal range is as follows:
- High AMH levels (greater than 4. 0 ng/ml): They could be manifestations of polycystic ovary syndrome (PCOS) or an increased number of antral follicles than usual. The hormone AMH is higher in women who have irregular or problems with ovulation; hence, natural conception may be impossible.
- Normal AMH levels (1. 0 to 4. 0 ng/ml): Women with levels within this range are likely to have a good ovarian reserve. They are likely to have a regular ovulation cycle hence they have improved chances of getting pregnant naturally or when they seek fertility solutions.
- Low AMH levels (less than 1. 0 ng/ml): Generally low AMH signifies the first aspect of poor ovarian reserve, meaning that the number of follicles left is lesser as compared to the age of the woman. This may mean the possibility of conceiving naturally is low and may have to ask for medical intervention like IVF.
How can the AMH levels be measured or reinvented?
A blood sample is used to conduct the test used to determine AMH levels and the procedure is not complicated at all. That is why AMH does not change during the menstrual cycle meaning that the test could be done at any time.
It is done most of the time together with fertility assessment and treatment, where a woman is advised to go for an AMH test. The outcomes of the test will then help the doctor to adjust treatment regimes based on the ovarian reserve of the woman in question.
That seems rather apparent but it is less obvious what it is that anti mullerian hormone levels tell us about fertility.
The levels of AMH provide information as to the ovarian reserve. Here is how different anti mullerian hormone levels can be interpreted in terms of fertility potential:
- High AMH Levels: receiving higher AMH values may mean a good rather than depleted ovarian reserve, however, extremely high AMH may be associated with polycystic ovary syndrome (PCOS). It is common for women with PCOS to have multiple immature follicles, and they either have low activity or do not ovulate at all (anovulation).
- Normal AMH Levels: A woman’s ability to conceive will be fine if her AMH level is within the normal limit for most women. This means the number of eggs in their reserve is adequate and hence will get good results in case they require fertility services. For a woman in this age bracket if she was facing issues with conceiving then it may not be because of poor ovarian reserve factor but because of other factors like fallopian tubes, the sperm or the uterus.
- Low AMH Levels: This means that if one has low anti mullerian hormone levels, then their chances of having many good eggs are limited. The medical term for this is the poor ovarian reserve. It is more often seen in women, especially those who are middle-aged, but it might be present in young women too. Even though AMH is low it is not necessarily impossible for a woman to become pregnant, but her chances of spontaneous conception as well as other fertility treatments will be lower. It would be essential to mention that some women with low AMH may have limited choice and might require IVF with donor eggs.
AMH Levels and IVF
In cases of women who are to be undergoing IVF, the AMH levels will have a hint of how the female will react to stimulation. High anti mullerian hormone levels suggest a woman will be likely to develop more follicles in response to stimulation as compared to a woman with low anti mullerian hormone levels who will be likely to develop few follicles.
Nevertheless, some implicit patterns were noted, According to which the more the number of eggs does not necessarily enhance the possibility of a pregnancy. The type of eggs also has a role and AMH testing is not the only means by which the fertility of a couple can be assessed. The goal and the purpose of the IVF process is to inseminate good quality, mature eggs that can result in the intended pregnancy.
Other Factors Affecting Fertility
Still, the arguments that have been presented above should make it easier to realize that AMH is not the sole indicator of fertility. It is also vital to recognize that fertility is not an exclusive gene pool but other features that may include a woman’s general health, hormonal balance, diet, and exercise routines can as well determine a woman’s fertility.
These sociological factors may further be classified under lifestyle factors wherein smoking obesity or chronic stress may further impact fertility.
Felicity: The Best Fertility Centre in Hyderabad
Anti Mullerian hormone (AMH) is an important marker of ovarian reserve and provides valuable insight into a woman’s fertility potential. Measuring AMH levels can help fertility specialists assess how many eggs remain in the ovaries, which is crucial when planning family-building strategies or pursuing fertility treatments like IVF.
At Felicity IVF, we understand how complex and emotionally challenging the journey to parenthood can be. That is why we take a personalised approach to fertility care, using AMH testing and other diagnostic tools to create tailored treatment plans that give you the best chance of success.
FAQS
AMH normal range is from 1.0 to 4.0 ng/ml, indicating a healthy ovarian reserve. Women with AMH levels within this range typically have a regular ovulation cycle and better chances of conceiving naturally or with fertility treatments.
Anti Müllerian Hormone levels help doctors predict how a woman will respond to ovarian stimulation in IVF. High AMH levels suggest more eggs can be retrieved, while low AMH levels may mean fewer eggs, requiring tailored treatment plans for success.
Couples with a history of genetic disorders, multiple miscarriages, or poor IVF outcomes should consider Pre Implantation Genetic Testing. It helps ensure the transfer of healthy embryos, increasing the chances of a healthy pregnancy.
